The Silent Liver Threat : Understanding and Combating Non-Alcoholic Steatohepatitis (NASH)
Non-Alcoholic Steatohepatitis (NASH) is a serious liver condition on the rise. Unlike its name suggests, NASH isn’t caused by alcohol but often linked to obesity, diabetes, and high cholesterol. This blog explores the causes, symptoms, diagnosis and treatment options, as well as the latest research aimed at combating this growing health challenge.
What is NASH?
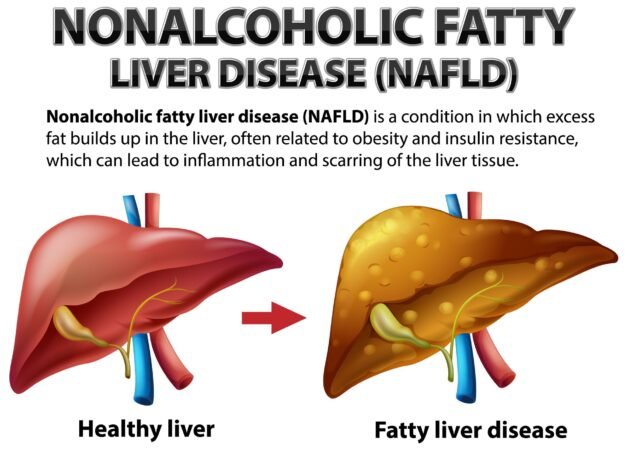
Non-Alcoholic Steatohepatitis (NASH) is a severe form of Non-Alcoholic Fatty Liver Disease, involving inflammation and liver cell damage that can progress to serious complications like fibrosis, cirrhosis and liver failure if left untreated (Younossi et al., 2018).. NASH is often asymptomatic in the early stages, making it difficult to diagnose until significant liver damage has occurred, which is a major concern.
The Rising Prevalence of NASH
The prevalence of NASH has been increasing alarmingly over the past few decades. According to a study published in the Journal of Hepatology, the global prevalence of NASH is estimated to be around 1.5% to 6.45% (Younossi et al., 2016). In the United States alone, it is estimated that about 3-12% of adults have NASH (Chalasani et al., 2018).
This rising trend is closely linked to the global obesity epidemic and the increasing prevalence of type 2 diabetes. As these conditions continue to affect more people worldwide, the incidence of NASH is expected to grow further.
Risk Factors and Causes
While the exact cause of NASH is not fully understood, several risk factors have been identified:
- Obesity: Excess body fat, especially around the waist, is strongly associated with NASH.
- Insulin Resistance and Type 2 Diabetes: These conditions affect how the body processes glucose and fats, contributing to fat accumulation in the liver.
- Metabolic Syndrome: This cluster of conditions, including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels, increases the risk of NASH (Friedman et al., 2018).
- Age and Gender: NASH is more common in people over 50 and tends to affect more women than men.
- Genetics: Some genetic variations may increase susceptibility to NASH.
The Progression from NAFLD to NASH
The progression from simple fatty liver (NAFLD) to NASH is complex and not fully elucidated. However, the “multiple hit hypothesis” is widely accepted in the scientific community. This theory suggests that multiple factors, including insulin resistance, oxidative stress, and inflammatory cytokines, work together to promote liver inflammation and damage (Buzzetti et al., 2016).
The first “hit” is the accumulation of fat in the liver, primarily due to insulin resistance. This makes the liver vulnerable to subsequent “hits,” which may include oxidative stress, mitochondrial dysfunction, and the release of inflammatory mediators. These factors collectively contribute to liver cell injury and the progression to NASH.
Symptoms and Diagnosis
As mentioned earlier, NASH often doesn’t present noticeable symptoms in its early stages. When symptoms do appear, they may include:
- Fatigue
- Pain or discomfort in the upper right abdomen
- Enlarged liver
- Enlarged blood vessels just beneath the skin’s surface
Diagnosing NASH can be challenging due to its asymptomatic nature in the early stages. Physicians typically use a combination of methods:
- Blood Tests: Liver function tests can indicate liver damage, although normal results don’t rule out NASH.
- Imaging Tests: Ultrasound, CT scans, or MRI can detect fat in the liver but can’t distinguish NASH from simple fatty liver.
- Liver Biopsy: This remains the gold standard for diagnosing NASH. It involves removing a small sample of liver tissue for examination under a microscope (European Association for the Study of the Liver et al., 2016).
Recent advancements in non-invasive diagnostic techniques, such as transient elastography (FibroScan) and magnetic resonance elastography, are showing promise in assessing liver fibrosis without the need for a biopsy (Castera et al., 2019).
Treatment Approaches
Currently, there is no FDA-approved medication specifically for NASH. However, treatment focuses on managing the underlying conditions and lifestyle modifications:
- Weight Loss: Losing 7-10% of body weight can significantly improve NASH and even reverse some liver damage (Vilar-Gomez et al., 2015).
- Diet Modification: A diet low in saturated fats and rich in fruits, vegetables, and whole grains is recommended.
- Exercise: Regular physical activity helps improve insulin sensitivity and reduce liver fat.
- Management of Comorbidities: Controlling diabetes, high cholesterol, and other metabolic conditions is crucial.
- Medications: While not specifically approved for NASH, some medications used for diabetes (like pioglitazone) and vitamin E have shown benefits in some patients with NASH (Chalasani et al., 2018).
Emerging Therapies and Future Directions
The field of NASH treatment is evolving rapidly, with numerous clinical trials underway. Some promising areas of research include:
- FXR Agonists: Drugs like obeticholic acid, which activate the farnesoid X receptor (FXR), have shown potential in improving liver fibrosis (Younossi et al., 2019).
- PPAR Agonists: These drugs, which target peroxisome proliferator-activated receptors, are being studied for their potential to improve insulin sensitivity and reduce liver fat.
- Anti-Fibrotic Agents: Compounds that directly target liver fibrosis are in various stages of clinical trials.
- Combination Therapies: Given the complex nature of NASH, combination therapies targeting multiple pathways are being explored.
The Role of Lifestyle in NASH Prevention and Management
While medical interventions are crucial, the importance of lifestyle changes in both preventing and managing NASH cannot be overstated. A study published in the New England Journal of Medicine demonstrated that lifestyle interventions resulting in weight loss could lead to NASH resolution in a significant proportion of patients (Vilar-Gomez et al., 2015).
Key lifestyle recommendations include:
- Maintaining a Healthy Weight: Even modest weight loss can have significant benefits.
- Following a Balanced Diet: The Mediterranean diet, in particular, has shown promise in improving NASH outcomes (Ryan et al., 2013).
- Regular Exercise: Both aerobic exercises and resistance training can help improve insulin sensitivity and reduce liver fat.
- Limiting Alcohol Consumption: While NASH is, by definition, not caused by alcohol, excessive alcohol consumption can exacerbate liver damage.
- Avoiding Unnecessary Medications: Some medications can strain the liver, so it’s important to use them judiciously under medical supervision.
The Global Impact of NASH
The rising prevalence of NASH has significant implications not just for individual health, but also for healthcare systems worldwide. A study published in Hepatology projected that the economic burden of NASH in the United States alone could reach $103 billion by 2030 (Younossi et al., 2016).
This economic impact, coupled with the potential for NASH to progress to more severe liver diseases, underscores the urgent need for increased awareness, early detection, and effective management strategies.
Conclusion
Non-Alcoholic Steatohepatitis represents a significant and growing challenge in global health. Its close association with obesity and metabolic syndrome means that its prevalence is likely to continue rising in the coming years. However, the increased focus on NASH in both clinical practice and research offers hope for better management and treatment options in the future.
As we await breakthrough therapies, the importance of lifestyle modifications in preventing and managing NASH cannot be overstated. By maintaining a healthy weight, following a balanced diet, and staying physically active, individuals can play a crucial role in safeguarding their liver health.
The fight against NASH requires a multifaceted approach, involving healthcare providers, researchers, policymakers, and individuals. With continued research, improved diagnostic tools, and a focus on preventive strategies, we can hope to turn the tide against this silent but significant threat to liver health.
Written by : Farokh Shabbir
References
Buzzetti, E., Pinzani, M., & Tsochatzis, E. A. (2016). The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism, 65(8), 1038-1048. https://doi.org/10.1016/j.metabol.2015.12.012
Castera, L., Friedrich-Rust, M., & Loomba, R. (2019). Noninvasive Assessment of Liver Disease in Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology, 156(5), 1264-1281.e4. https://doi.org/10.1053/j.gastro.2018.12.036
Chalasani, N., Younossi, Z., Lavine, J. E., Charlton, M., Cusi, K., Rinella, M., Harrison, S. A., Brunt, E. M., & Sanyal, A. J. (2018). The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology, 67(1), 328-357. https://doi.org/10.1002/hep.29367
European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), & European Association for the Study of Obesity (EASO). (2016). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. Journal of Hepatology, 64(6), 1388-1402. https://doi.org/10.1016/j.jhep.2015.11.004
Friedman, S. L., Neuschwander-Tetri, B. A., Rinella, M., & Sanyal, A. J. (2018). Mechanisms of NAFLD development and therapeutic strategies. Nature Medicine, 24(7), 908-922. https://doi.org/10.1038/s41591-018-0104-9
Ryan, M. C., Itsiopoulos, C., Thodis, T., Ward, G., Trost, N., Hofferberth, S., O’Dea, K., Desmond, P. V., Johnson, N. A., & Wilson, A. M. (2013). The Mediterranean diet improves hepatic steatosis and insulin sensitivity in individuals with non-alcoholic fatty liver disease. Journal of Hepatology, 59(1), 138-143. https://doi.org/10.1016/j.jhep.2013.02.012
Vilar-Gomez, E., Martinez-Perez, Y., Calzadilla-Bertot, L., Torres-Gonzalez, A., Gra-Oramas, B., Gonzalez-Fabian, L., Friedman, S. L., Diago, M., & Romero-Gomez, M. (2015). Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology, 149(2), 367-378.e5. https://doi.org/10.1053/j.gastro.2015.04.005
Younossi, Z. M., Koenig, A. B., Abdelatif, D., Fazel, Y., Henry, L., & Wymer, M. (2016). Global epidemiology of nonalcoholic fatty liver disease—Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology, 64(1), 73-84. https://doi.org/10.1002/hep.28431
Younossi, Z. M., Blissett, D., Blissett, R., Henry, L., Stepanova, M., Younossi, Y., Racila, A., Hunt, S., & Beckerman, R. (2016). The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology, 64(5), 1577-1586. https://doi.org/10.1002/hep.28785
Younossi, Z., Tacke, F., Arrese, M., Chander Sharma, B., Mostafa, I., Bugianesi, E., Wai-Sun Wong, V., Yilmaz, Y., George, J., Fan, J., & Vos, M. B. (2019). Global Perspectives on Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis. Hepatology, 69(6), 2672-2682. https://doi.org/10.1002/hep.30251