Insulin Resistance
In today’s fast-paced world, where convenience foods and sedentary lifestyles have become the norm, a silent epidemic is sweeping across nations. Insulin resistance, a condition that disrupts the body’s ability to effectively use insulin, has emerged as a critical factor in the development of various metabolic disorders. This blog post delves into the intricacies of insulin resistance, exploring its causes, consequences and potential strategies for prevention and management.
Understanding Insulin and Its Role
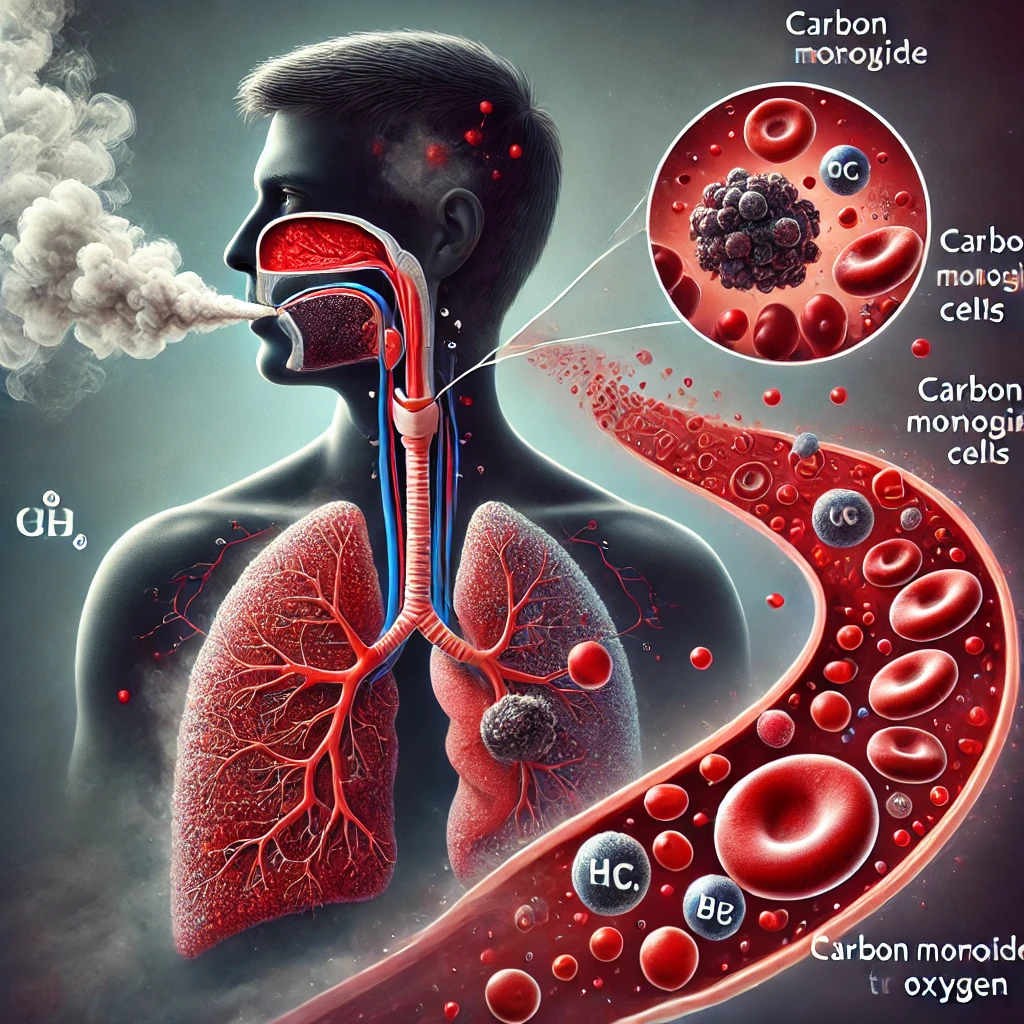
Before we dive into insulin resistance, it’s crucial to understand the role of insulin in our bodies. Insulin is a hormone produced by the pancreas that acts as a key, unlocking cells to allow glucose from the bloodstream to enter and be used for energy. This process is vital for maintaining stable blood sugar levels and ensuring proper energy utilization throughout the body (American Diabetes Association [ADA], 2022).
What is Insulin Resistance?
Insulin resistance occurs when cells in the muscles, fat, and liver don’t respond well to insulin and can’t easily take up glucose from the blood. As a result, the pancreas produces more insulin to help glucose enter the cells. Over time, this can lead to prediabetes or type 2 diabetes as the pancreas fails to keep up with the increased demand for insulin (National Institute of Diabetes and Digestive and Kidney Diseases [NIDDK], 2023).
The Prevalence of Insulin Resistance
The exact prevalence of insulin resistance is challenging to determine, as it often goes undiagnosed in its early stages. However, it’s estimated that up to 40% of adults in the United States may have some degree of insulin resistance (Sah et al., 2016). This high prevalence underscores the importance of understanding and addressing this condition.
Causes and Risk Factors
Several factors contribute to the development of insulin resistance:
- Obesity: Excess body fat, particularly around the waist, is strongly associated with insulin resistance. Adipose tissue releases inflammatory markers and free fatty acids that interfere with insulin signaling (Ye, 2013).
- Physical Inactivity: A sedentary lifestyle reduces muscle glucose uptake and insulin sensitivity. Regular physical activity helps maintain insulin sensitivity by promoting glucose uptake in muscles (Colberg et al., 2016).
- Diet: Diets high in refined carbohydrates, saturated fats, and added sugars can contribute to insulin resistance. Conversely, a diet rich in fiber, whole grains, and healthy fats may improve insulin sensitivity (Guess et al., 2016).
- Genetics: Some genetic factors can predispose individuals to insulin resistance. However, lifestyle factors often play a more significant role in its development (Scott et al., 2014).
- Chronic Stress: Prolonged stress can lead to elevated cortisol levels, which may interfere with insulin function and promote insulin resistance (Magomedova & Cummins, 2016).
- Sleep Deprivation: Inadequate sleep or poor sleep quality has been linked to impaired glucose metabolism and insulin resistance (Reutrakul & Van Cauter, 2018).
The Consequences of Insulin Resistance
Insulin resistance is not just a precursor to type 2 diabetes; it’s associated with a range of health issues:
- Metabolic Syndrome: Insulin resistance is a key component of metabolic syndrome, a cluster of conditions including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels (Saklayen, 2018).
- Cardiovascular Disease: Insulin resistance is associated with an increased risk of heart disease and stroke (Ormazabal et al., 2018).
- Non-Alcoholic Fatty Liver Disease (NAFLD): Insulin resistance plays a crucial role in the development and progression of NAFLD, which can lead to liver inflammation and fibrosis (Kitade et al., 2017).
- Polycystic Ovary Syndrome (PCOS): Many women with PCOS have insulin resistance, which can exacerbate hormonal imbalances and fertility issues (Diamanti-Kandarakis & Dunaif, 2012).
- Certain Cancers: Insulin resistance has been linked to an increased risk of certain cancers, including colorectal, breast, and endometrial cancer (Orgel & Mittelman, 2013).
Diagnosing Insulin Resistance
Detecting insulin resistance in its early stages can be challenging, as there’s no single definitive test. However, healthcare providers may use a combination of the following to assess insulin sensitivity:
- Fasting Plasma Glucose Test: Measures blood sugar levels after an 8-hour fast.
- Oral Glucose Tolerance Test (OGTT): Evaluates how the body processes glucose over a 2-hour period after consuming a glucose-rich drink.
- Homeostatic Model Assessment of Insulin Resistance (HOMA-IR): A mathematical model that estimates insulin resistance using fasting glucose and insulin levels.
- Hyperinsulinemic-Euglycemic Clamp: Considered the gold standard for measuring insulin sensitivity, though it’s primarily used in research settings due to its complexity (Wallace et al., 2004).
Strategies for Prevention and Management
The good news is that insulin resistance is often preventable and manageable through lifestyle modifications:
- Regular Physical Activity: Engaging in at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week can significantly improve insulin sensitivity (Colberg et al., 2016).
- Healthy Diet: Adopting a diet rich in whole grains, lean proteins, fruits, vegetables, and healthy fats can help improve insulin sensitivity. The Mediterranean diet and the DASH (Dietary Approaches to Stop Hypertension) diet have shown promising results in managing insulin resistance (Esposito et al., 2015).
- Weight Management: Losing even a modest amount of weight (5-10% of body weight) can lead to significant improvements in insulin sensitivity for overweight or obese individuals (Magkos et al., 2016).
- Stress Reduction: Incorporating stress-management techniques such as meditation, yoga, or deep breathing exercises can help mitigate the negative effects of chronic stress on insulin sensitivity (Pascoe et al., 2017).
- Adequate Sleep: Aiming for 7-9 hours of quality sleep per night can help maintain proper glucose metabolism and insulin sensitivity (Reutrakul & Van Cauter, 2018).
- Medications: In some cases, healthcare providers may prescribe medications like metformin to improve insulin sensitivity, particularly for individuals at high risk of developing type 2 diabetes (ADA, 2022).
Emerging Research and Future Directions
The field of insulin resistance research is rapidly evolving, with new insights emerging regularly:
- Gut Microbiome: Recent studies suggest that the composition of gut bacteria may influence insulin sensitivity. Probiotics and prebiotics are being investigated as potential interventions (Vallianou et al., 2019).
- Chronobiology: The timing of meals and sleep-wake cycles (circadian rhythms) appears to play a role in insulin sensitivity. Time-restricted feeding and chrononutrition are areas of active research (Stenvers et al., 2019).
- Personalized Medicine: Advances in genomics and metabolomics are paving the way for more personalized approaches to preventing and managing insulin resistance based on individual genetic and metabolic profiles (Fitipaldi et al., 2018).
- Novel Pharmacological Approaches: Researchers are exploring new drug targets and mechanisms to improve insulin sensitivity, including SGLT2 inhibitors and incretin mimetics (DeFronzo et al., 2015).
Conclusion
Insulin resistance is a complex condition that sits at the crossroads of metabolism, nutrition, and lifestyle. As our understanding of its mechanisms deepens, so too does our ability to prevent and manage this silent threat to metabolic health. By adopting a proactive approach that combines regular physical activity, a balanced diet, stress management, and adequate sleep, we can take significant steps toward improving insulin sensitivity and overall health.
As research continues to unravel the intricacies of insulin resistance, it’s clear that a multifaceted approach is necessary to address this growing public health concern. By staying informed and making conscious lifestyle choices, we can work towards a future where insulin resistance no longer poses such a significant threat to global health.
Written by : Farokh Shabbir
References
American Diabetes Association. (2022). Standards of Medical Care in Diabetes—2022. Diabetes Care, 45(Supplement 1), S1-S264.
Colberg, S. R., Sigal, R. J., Yardley, J. E., Riddell, M. C., Dunstan, D. W., Dempsey, P. C., … & Tate, D. F. (2016). Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care, 39(11), 2065-2079.
DeFronzo, R. A., Norton, L., & Abdul-Ghani, M. (2015). Renal, metabolic and cardiovascular considerations of SGLT2 inhibition. Nature Reviews Nephrology, 11(11), 385-399.
Diamanti-Kandarakis, E., & Dunaif, A. (2012). Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocrine Reviews, 33(6), 981-1030.
Esposito, K., Maiorino, M. I., Bellastella, G., Chiodini, P., Panagiotakos, D., & Giugliano, D. (2015). A journey into a Mediterranean diet and type 2 diabetes: a systematic review with meta-analyses. BMJ Open, 5(8), e008222.
Fitipaldi, H., McCarthy, M. I., Florez, J. C., & Franks, P. W. (2018). A global overview of precision medicine in type 2 diabetes. Diabetes, 67(10), 1911-1922.
Guess, N. D., Dornhorst, A., Oliver, N., & Frost, G. S. (2016). A randomized controlled trial: the effect of inulin on weight management and ectopic fat in subjects with prediabetes. Nutrition & Metabolism, 13(1), 1-10.
Kitade, H., Chen, G., Ni, Y., & Ota, T. (2017). Nonalcoholic fatty liver disease and insulin resistance: new insights and potential new treatments. Nutrients, 9(4), 387.
Magkos, F., Fraterrigo, G., Yoshino, J., Luecking, C., Kirbach, K., Kelly, S. C., … & Klein, S. (2016). Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metabolism, 23(4), 591-601.
Magomedova, L., & Cummins, C. L. (2016). Glucocorticoids and metabolic control. Handbook of Experimental Pharmacology, 233, 73-93.
National Institute of Diabetes and Digestive and Kidney Diseases. (2023). Insulin Resistance & Prediabetes. Retrieved from https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance
Orgel, E., & Mittelman, S. D. (2013). The links between insulin resistance, diabetes, and cancer. Current Diabetes Reports, 13(2), 213-222.
Ormazabal, V., Nair, S., Elfeky, O., Aguayo, C., Salomon, C., & Zuñiga, F. A. (2018). Association between insulin resistance and the development of cardiovascular disease. Cardiovascular Diabetology, 17(1), 1-14.
Pascoe, M. C., Thompson, D. R., Jenkins, Z. M., & Ski, C. F. (2017). Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. Journal of Psychiatric Research, 95, 156-178.
Reutrakul, S., & Van Cauter, E. (2018). Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism, 84, 56-66.
Sah, S. P., Singh, B., Choudhary, S., & Kumar, A. (2016). Animal models of insulin resistance: A review. Pharmacological Reports, 68(6), 1165-1177.
Saklayen, M. G. (2018). The global epidemic of the metabolic syndrome. Current Hypertension Reports, 20(2), 12.
Scott, R. A., Fall, T., Pasko, D., Barker, A., Sharp, S. J., Arriola, L., … & Langenberg, C. (2014). Common genetic variants highlight the role of insulin resistance and body fat distribution in type 2 diabetes, independent of obesity. Diabetes, 63(12), 4378-4387.
Stenvers, D. J., Scheer, F. A., Schrauwen, P., la Fleur, S. E., & Kalsbeek, A. (2019). Circadian clocks and insulin resistance. Nature Reviews Endocrinology, 15(2), 75-89.
Vallianou, N. G., Stratigou, T., & Tsagarakis, S. (2019). Microbiome and diabetes: Where are we now? Diabetes Research and Clinical Practice, 146, 111-118.
Wallace, T. M., Levy, J. C., & Matthews, D. R. (2004). Use and abuse of HOMA modeling. Diabetes Care, 27(6), 1487-1495.
Ye, J. (2013). Mechanisms of insulin resistance in obesity. Frontiers of Medicine, 7(1), 14-24.