Managing Diarrhea : Tips for Relief and Prevention
Diarrhea is a common gastrointestinal condition that affects millions of people worldwide. While often viewed as a mere inconvenience, it can lead to severe complications if left untreated, especially in vulnerable populations. This comprehensive guide delves into the causes, symptoms, treatments, and prevention strategies for diarrhea, providing you with the knowledge to manage this condition effectively.
What is Diarrhea?
It is characterized by loose, watery stools occurring more frequently than usual. It’s typically defined as having three or more loose bowel movements in a 24-hour period (World Health Organization [WHO], 2017). While most cases of diarrhea resolve on their own within a few days, persistent or severe cases can lead to dehydration and other complications.
Causes of Diarrhea
It can can result from various factors, including:
- Infections: Viral, bacterial, or parasitic infections are common causes of acute diarrhea. Rotavirus, norovirus, Escherichia coli (E. coli), Salmonella, and Giardia are frequent culprits (Centers for Disease Control and Prevention [CDC], 2021).
- Food intolerances: Lactose intolerance, fructose malabsorption, and celiac disease can trigger diarrhea when consuming specific foods (National Institute of Diabetes and Digestive and Kidney Diseases [NIDDK], 2016).
- Medications: Antibiotics, antacids containing magnesium, and some cancer treatments can disrupt the gut microbiome, leading to diarrhea (Mayo Clinic, 2021).
- Digestive disorders: Conditions such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and microscopic colitis can cause chronic diarrhea (Schiller et al., 2017).
- Stress and anxiety: Psychological factors can influence gut motility and secretion, potentially triggering diarrhea (Qin et al., 2014).
Symptoms and Complications of Diarrhea
The primary symptom of diarrhea is loose, watery stools. However, it may be accompanied by:
- Abdominal cramps or pain
- Nausea and vomiting
- Fever
- Blood in the stool
- Bloating
- Urgent need to have a bowel movement
The most significant complication of diarrhea is dehydration, which can be life-threatening, especially in young children and older adults. Signs of dehydration include:
- Extreme thirst
- Dry mouth and skin
- Little or no urination
- Weakness and dizziness
- Rapid heartbeat
In severe cases, diarrhea can lead to electrolyte imbalances, kidney problems, and even death if left untreated (WHO, 2017).
Diagnosis of Diarrhea
Most cases of acute diarrhea don’t require extensive diagnostic procedures. However, if symptoms persist or are severe, a healthcare provider may recommend:
- Stool tests: To identify bacterial, viral, or parasitic infections.
- Blood tests: To check for signs of infection or other underlying conditions.
- Colonoscopy or sigmoidoscopy: For chronic diarrhea, to examine the colon for abnormalities.
- Hydrogen breath tests: To diagnose lactose intolerance or small intestinal bacterial overgrowth (SIBO).
Treatment Approaches
The primary goal in treating diarrhea is preventing dehydration. Treatment strategies include:
- Fluid replacement: Oral rehydration solutions (ORS) are crucial in replacing lost fluids and electrolytes. In severe cases, intravenous fluids may be necessary (WHO, 2017).
- Dietary changes: The BRAT diet (Bananas, Rice, Applesauce, Toast) can help firm up stools and provide easily digestible nutrients (NIDDK, 2016).
- Probiotics: Some studies suggest that probiotics, particularly Lactobacillus GG and Saccharomyces boulardii, may help reduce the duration of infectious diarrhea (Szajewska et al., 2019).
- Medications:
- Bismuth subsalicylate (Pepto-Bismol) can help relieve symptoms.
- Loperamide (Imodium) can reduce the frequency of bowel movements but should be used cautiously in infectious diarrhea.
- Antibiotics may be prescribed for bacterial infections.
- Addressing underlying conditions: For chronic diarrhea, treating the underlying cause (e.g., IBD, celiac disease) is essential.
It’s important to note that antidiarrheal medications should not be given to young children without medical supervision, as they can lead to complications in certain infectious causes of diarrhea (CDC, 2021).
Prevention Strategies
Preventing diarrhea involves several key practices:
- Hand hygiene: Proper handwashing, especially before handling food and after using the bathroom, is crucial in preventing the spread of infectious agents (CDC, 2021).
- Food safety: Properly cooking foods, especially meats, and avoiding contaminated water can prevent many cases of foodborne diarrhea (WHO, 2017).
- Vaccinations: Rotavirus vaccines have significantly reduced severe diarrhea in children in many countries (Tate et al., 2016).
- Safe water practices: In areas with unsafe water supplies, boiling or treating water before consumption is essential.
- Breastfeeding: For infants, exclusive breastfeeding for the first six months of life can reduce the risk of diarrheal diseases (WHO, 2017).
Special Considerations for Different Populations
Children
Diarrhea remains a leading cause of death in children under five years old, particularly in developing countries. Prompt treatment with ORS is crucial. The WHO and UNICEF recommend zinc supplementation along with ORS for children with acute diarrhea, as it can reduce the severity and duration of the illness (WHO/UNICEF, 2004).
Older Adults
Older adults are more susceptible to severe complications from diarrhea due to age-related changes in the digestive system and potential underlying health conditions. They may also be at higher risk of medication-induced diarrhea due to polypharmacy (Schiller et al., 2017).
Travelers
Traveler’s diarrhea affects 20-50% of international travelers, depending on the destination. Preventive measures include avoiding tap water, raw fruits and vegetables, and unpasteurized dairy products in high-risk areas. Some studies suggest that bismuth subsalicylate can be used prophylactically for short trips (Steffen et al., 2015).
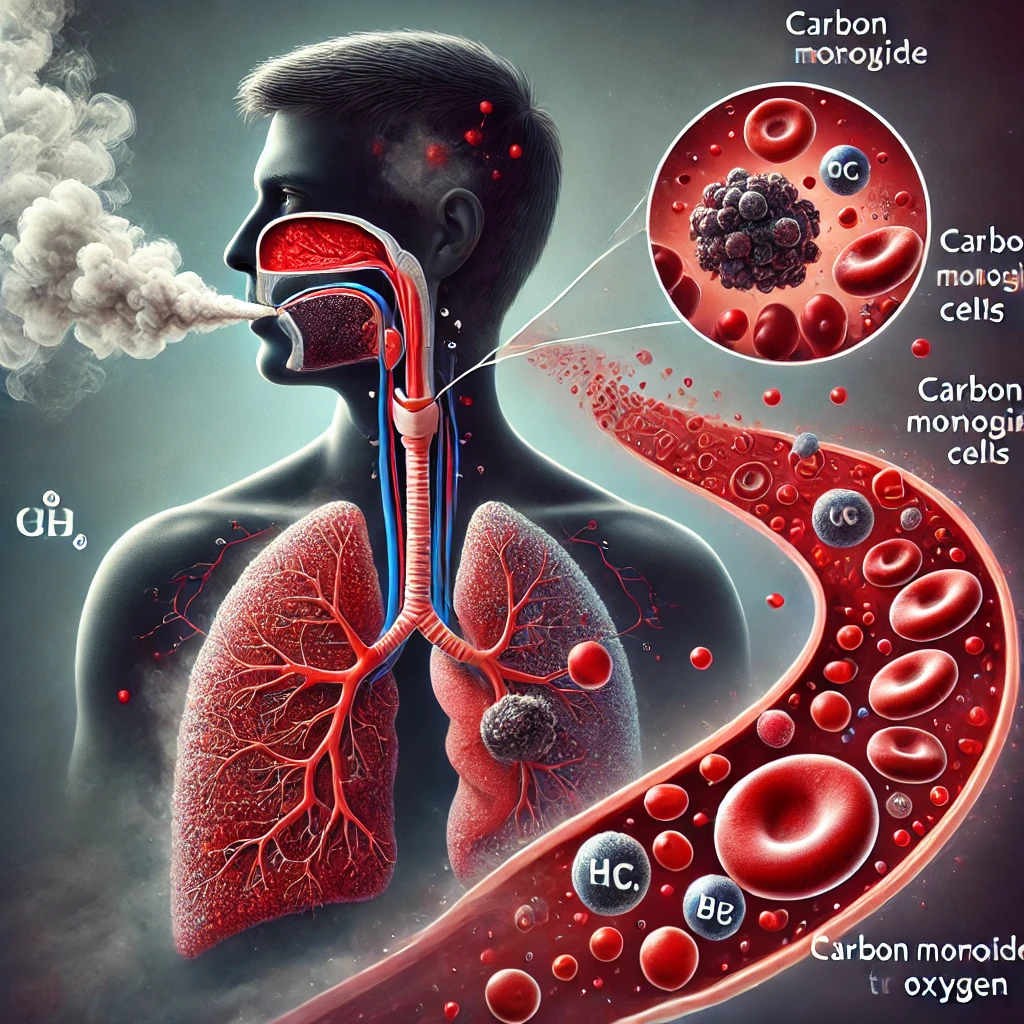
The Role of the Gut Microbiome
Recent research has highlighted the importance of the gut microbiome in diarrheal diseases. The complex ecosystem of microorganisms in our intestines plays a crucial role in digestion, immunity, and protection against pathogens. Disruptions to this microbiome, whether from infections, antibiotics, or dietary changes, can contribute to diarrhea (Lynch & Pedersen, 2016).
Emerging treatments, such as fecal microbiota transplantation (FMT), have shown promise in treating recurrent Clostridioides difficile infections, a severe form of antibiotic-associated diarrhea. While more research is needed, this approach underscores the potential of microbiome-based therapies in managing diarrheal diseases (Staley et al., 2019).
Global Health Implications
Diarrheal diseases remain a significant global health challenge, particularly in low- and middle-income countries. They are the second leading cause of death in children under five years old, responsible for approximately 525,000 deaths annually (WHO, 2017). Improving access to clean water, sanitation, and healthcare services is crucial in reducing this burden.
The Sustainable Development Goals (SDGs) set by the United Nations include targets related to reducing waterborne diseases and improving water and sanitation infrastructure, which are directly relevant to preventing diarrheal diseases (United Nations, 2015).
Conclusion
Diarrhea, while common, should not be taken lightly. Understanding its causes, recognizing its symptoms, and knowing when to seek medical attention are crucial for effective management. By implementing preventive measures and responding promptly to symptoms, we can significantly reduce the impact of this condition on individuals and communities.
As research continues to uncover new insights into the gut microbiome and novel treatment approaches, our ability to prevent and manage diarrheal diseases will likely improve. In the meantime, basic hygiene practices, access to clean water and sanitation, and prompt treatment remain our best defenses against this pervasive health challenge.
Written by : Farokh Shabbir
References
- Centers for Disease Control and Prevention (CDC). (2021). Diarrhea.
- Lynch, S. V., & Pedersen, O. (2016). The Human Intestinal Microbiome in Health and Disease. New England Journal of Medicine, 375(24), 2369-2379.
- Mayo Clinic. (2021). Diarrhea.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
- Qin, H. Y., Cheng, C. W., Tang, X. D., & Bian, Z. X. (2014). Impact of psychological stress on irritable bowel syndrome. World Journal of Gastroenterology, 20(39), 14126-14131.
- Schiller, L. R., Pardi, D. S., & Sellin, J. H. (2017). Chronic Diarrhea: Diagnosis and Management. Clinical Gastroenterology and Hepatology, 15(2), 182-193.
- Staley, C., Khoruts, A., & Sadowsky, M. J. (2019). Contemporary Applications of Fecal Microbiota Transplantation to Treat Intestinal Diseases in Humans. Archives of Medical Research, 50(8), 576-587.
- Steffen, R., Hill, D. R., & DuPont, H. L. (2015). Traveler’s diarrhea: a clinical review. JAMA, 313(1), 71-80.
- Szajewska, H., Kołodziej, M., Gieruszczak-Białek, D., Skórka, A., Ruszczyński, M., & Shamir, R. (2019). Systematic review with meta-analysis: Lactobacillus rhamnosus GG for treating acute gastroenteritis in children – a 2019 update. Alimentary Pharmacology & Therapeutics, 49(11), 1376-1384.
- Tate, J. E., Burton, A. H., Boschi-Pinto, C., & Parashar, U. D. (2016). Global, Regional, and National Estimates of Rotavirus Mortality in Children <5 Years of Age, 2000-2013. Clinical Infectious Diseases, 62(suppl_2), S96-S105.
- United Nations. (2015). Sustainable Development Goals. Retrieved from [UN website].
- World Health Organization (WHO). (2017). Diarrhoeal disease. Retrieved from [WHO website].
- World Health Organization/UNICEF. (2004). Clinical Management of Acute Diarrhoea: WHO/UNICEF Joint Statement. Retrieved from [WHO/UNICEF website].