Breathing Easy : Unraveling the Mysteries of Asthma in the Modern World
Asthma, a chronic respiratory condition affecting millions worldwide, has been a subject of intense research and discussion in recent years. As our understanding of this complex disease evolves, so do the strategies for managing and treating it. This blog post delves into the current state of asthma knowledge, exploring its causes, symptoms, diagnosis, treatment options, and the latest advancements in asthma care.
Understanding Asthma: More Than Just Shortness of Breath
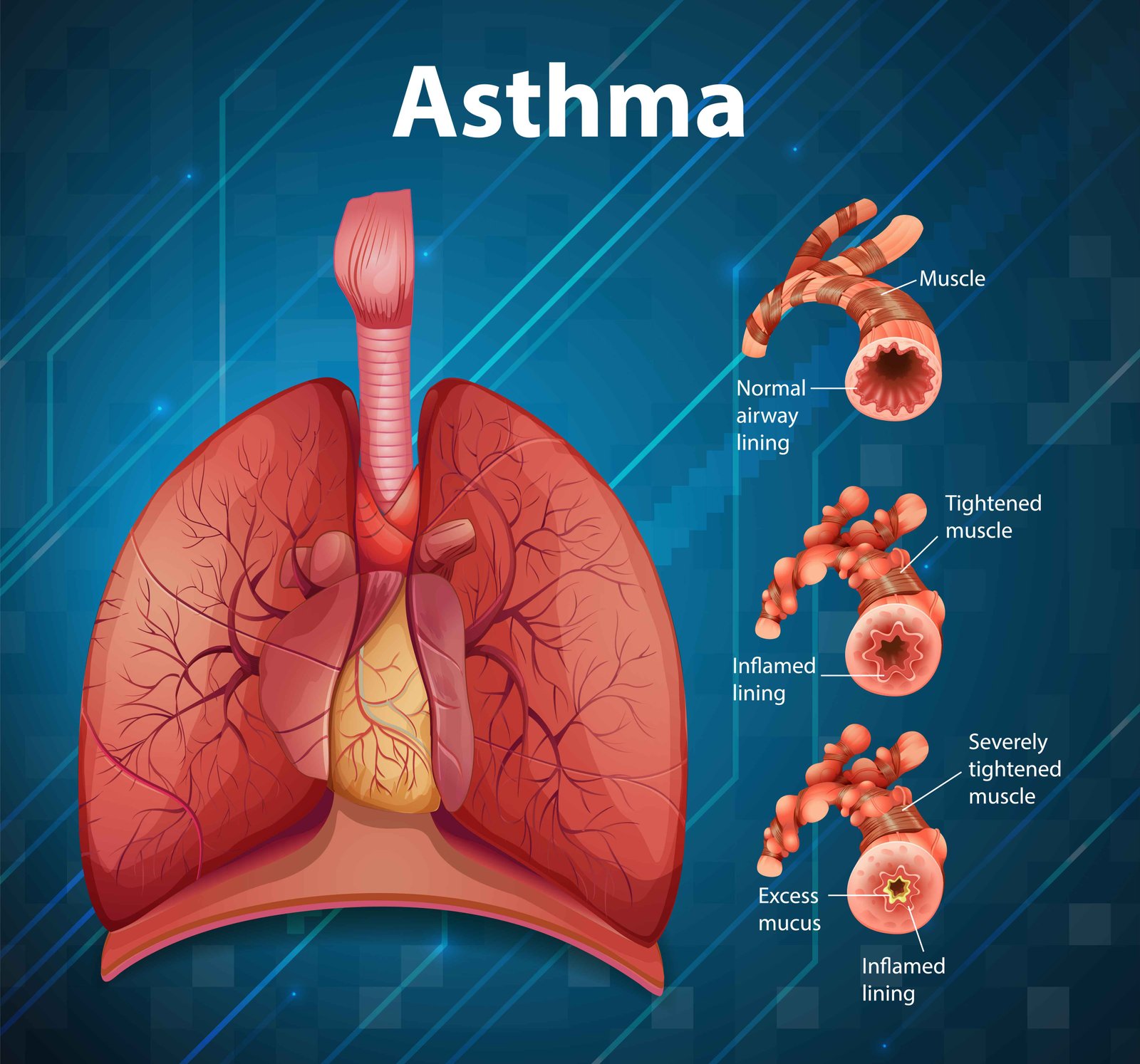
It is characterized by inflammation and narrowing of the airways, leading to symptoms such as wheezing, coughing, chest tightness, and shortness of breath. While these symptoms are well-known, the underlying mechanisms of this disease are far more complex than previously thought. Recent research has shed light on the intricate interplay between genetic predisposition and environmental factors in the development and progression of this disease (Holgate et al., 2015).
The heterogeneity of respiratory condition is now widely recognized, with different phenotypes and endotypes identified. This understanding has paved the way for more personalized approaches to respiratory condition management, moving beyond the one-size-fits-all treatment models of the past (Wenzel, 2012).
The Rising Tide: Asthma Prevalence and Risk Factors
Global respiratory condition prevalence has been on the rise, with an estimated 339 million people affected worldwide as of 2016 (Global Asthma Network, 2018). This increase has been attributed to various factors, including urbanization, air pollution, and changes in lifestyle and diet.
Environmental triggers play a crucial role in respiratory condition exacerbations. Common triggers include:
- Allergens (e.g., dust mites, pollen, animal dander)
- Air pollutants (both indoor and outdoor)
- Respiratory infections
- Physical activity
- Stress and strong emotions
Understanding and managing these triggers is essential for effective respiratory condition control. Recent studies have also highlighted the role of early-life exposures in shaping respiratory condition risk, emphasizing the importance of preventive strategies during pregnancy and early childhood (Platts-Mills, 2015).
Diagnosis: Beyond the Wheeze
Diagnosing chronic respiratory condition has traditionally relied on a combination of clinical history, physical examination, and lung function tests. However, the limitations of these methods in capturing the full spectrum of respiratory condition phenotypes have become apparent. New diagnostic tools and biomarkers are emerging to provide a more comprehensive picture of an individual’s asthma status.
Fractional exhaled nitric oxide (FeNO) testing has gained traction as a non-invasive method to assess airway inflammation. This test can help identify eosinophilic inflammation, a key feature of certain respiratory condition phenotypes, and guide treatment decisions (Dweik et al., 2011).
Additionally, advances in imaging technologies, such as hyperpolarized gas MRI, offer unprecedented insights into regional lung ventilation and small airway function in respiratory condition patients (Svenningsen et al., 2013). These novel diagnostic approaches promise to enhance our ability to tailor treatments to individual patients.
Treatment Landscape: From Rescue Inhalers to Biologics
The management of respiratory condition has seen significant advancements in recent years. While inhaled corticosteroids (ICS) and long-acting beta-agonists (LABAs) remain the cornerstone of respiratory condition treatment, new targeted therapies are revolutionizing care for patients with severe or difficult-to-treat respiratory condition .
Biologic therapies, such as anti-IgE (omalizumab), anti-IL-5 (mepolizumab, reslizumab), and anti-IL-4/IL-13 (dupilumab) antibodies, have shown remarkable efficacy in reducing exacerbations and improving quality of life for patients with specific respiratory condition phenotypes (Farne et al., 2017). These targeted treatments underscore the importance of precise phenotyping in respiratory condition management.
Moreover, the advent of smart inhalers and digital health technologies is transforming how patients and healthcare providers monitor and manage respiratory condition . These devices can track medication adherence, provide real-time feedback, and even predict exacerbations based on usage patterns and environmental data (Chan et al., 2013).
The Role of Lifestyle: Beyond Medication
While pharmacological interventions are crucial, the importance of lifestyle modifications in respiratory condition management cannot be overstated. Recent research has highlighted the potential benefits of dietary interventions, exercise, and stress reduction techniques in improving asthma outcomes.
A Mediterranean diet, rich in fruits, vegetables, and omega-3 fatty acids, has been associated with improved respiratory condition control and reduced risk of exacerbations (Barros et al., 2017). Regular physical activity, when properly managed, can improve lung function and overall quality of life for respiratory condition patients (Carson et al., 2013).
Mindfulness-based stress reduction techniques have also shown promise in reducing asthma-related stress and improving quality of life (Pbert et al., 2012). These non-pharmacological approaches offer complementary strategies to enhance respiratory condition management and empower patients to take an active role in their care.
The Asthma-Obesity Connection: A Growing Concern
The rising prevalence of obesity has brought attention to its complex relationship with respiratory condition . Obese individuals are not only at higher risk of developing asthma but also tend to have more severe symptoms and poorer response to standard treatments (Dixon et al., 2010).
The mechanisms underlying this association are multifaceted, involving mechanical, inflammatory, and metabolic factors. Weight loss interventions have been shown to improve respiratory condition control and quality of life in obese patients with asthma, highlighting the importance of addressing this comorbidity in comprehensive asthma care (Dias-Júnior et al., 2014).
Pediatric Asthma: Unique Challenges and Opportunities
respiratory condition in children presents unique challenges, from diagnosis to long-term management. Early intervention is crucial, as childhood asthma can have lasting impacts on lung function and overall health into adulthood.
Recent guidelines emphasize the importance of assessing and addressing environmental exposures in pediatric asthma management (Matsui et al., 2016). School-based interventions and education programs have shown promise in improving asthma outcomes for children, particularly in underserved communities (Cicutto et al., 2013).
The concept of the “asthma predictive index” has been refined to help identify children at high risk of persistent asthma, allowing for earlier intervention and potentially altering the course of the disease (Castro-Rodriguez et al., 2011).
The Future of Asthma Care: Precision Medicine and Beyond
As we look to the future, the field of respiratory condition research and treatment is poised for significant advancements. The promise of precision medicine, leveraging genetic, molecular, and clinical data to tailor treatments to individual patients, is becoming a reality in asthma care.
Emerging areas of research include:
- Microbiome studies: Investigating the role of the lung and gut microbiome in respiratory condition development and progression (Huang & Boushey, 2015).
- Epigenetics: Exploring how environmental factors influence gene expression in asthma (DeVries & Vercelli, 2013).
- Artificial intelligence: Developing predictive models for respiratory condition exacerbations and treatment responses (Bos et al., 2017).
- Novel drug delivery systems: Improving the efficacy and reducing side effects of asthma medications (Stein & Thiel, 2017).
These cutting-edge approaches hold the potential to transform our understanding and management of asthma in the coming years.
Conclusion: A Breath of Fresh Air in Asthma Care
As our knowledge of respiratory condition expands, so does our ability to provide more effective, personalized care to those affected by this complex condition. From advanced diagnostics and targeted therapies to lifestyle interventions and digital health solutions, the landscape of asthma management is evolving rapidly.
While challenges remain, particularly in addressing health disparities and improving access to care, the future of respiratory condition treatment looks promising. By embracing a holistic, patient-centered approach that combines the latest scientific advancements with compassionate care, we can help individuals with asthma breathe easier and live fuller lives.
As research continues to unravel the mysteries of asthma, one thing is clear: the key to better outcomes lies in a collaborative effort between patients, healthcare providers, researchers, and policymakers. Together, we can work towards a future where asthma is no longer a barrier to a full and active life.
Written by : Farokh Shabbir
References
Bos, L. D., Vijverberg, S. J., Brinkman, P., Hekking, P. P., Rutjes, N. W., Zariwala, M. A., … & Sterk, P. J. (2017). Machine learning for prediction of exacerbations in patients with adult-onset asthma. The Journal of Allergy and Clinical Immunology, 140(4), 1169-1171.
Castro-Rodriguez, J. A., Holberg, C. J., Wright, A. L., & Martinez, F. D. (2011). A clinical index to define risk of asthma in young children with recurrent wheezing. American Journal of Respiratory and Critical Care Medicine, 162(4), 1403-1406.
Chan, A. H., Reddel, H. K., Apter, A., Eakin, M., Riekert, K., & Foster, J. M. (2013). Adherence monitoring and e-health: how clinicians and researchers can use technology to promote inhaler adherence for asthma. The Journal of Allergy and Clinical Immunology: In Practice, 1(5), 446-454.
Cicutto, L., To, T., & Murphy, S. (2013). A randomized controlled trial of a public health nurse‐delivered asthma program to elementary schools. Journal of School Health, 83(12), 876-884.
DeVries, A., & Vercelli, D. (2013). Epigenetics of human asthma and allergy: promises to keep. Asian Pacific Journal of Allergy and Immunology, 31(3), 183.
Dixon, A. E., Holguin, F., Sood, A., Salome, C. M., Pratley, R. E., Beuther, D. A., … & Shore, S. A. (2010). An official American Thoracic Society Workshop report: obesity and asthma. Proceedings of the American Thoracic Society, 7(5), 325-335.
Dweik, R. A., Boggs, P. B., Erzurum, S. C., Irvin, C. G., Leigh, M. W., Lundberg, J. O., … & Taylor, D. R. (2011). An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. American Journal of Respiratory and Critical Care Medicine, 184(5), 602-615.
Farne, H. A., Wilson, A., Powell, C., Bax, L., & Milan, S. J. (2017). Anti‐IL5 therapies for asthma. Cochrane Database of Systematic Reviews, (9).
Global Asthma Network. (2018). The Global Asthma Report 2018. Auckland, New Zealand: Global Asthma Network.
Holgate, S. T., Wenzel, S., Postma, D. S., Weiss, S. T., Renz, H., & Sly, P. D. (2015). Asthma. Nature Reviews Disease Primers, 1(1), 1-22.
Huang, Y. J., & Boushey, H. A. (2015). The microbiome in asthma. Journal of Allergy and Clinical Immunology, 135(1), 25-30.
Matsui, E. C., Abramson, S. L., & Sandel, M. T. (2016). Indoor environmental control practices and asthma management. Pediatrics, 138(5).
Pbert, L., Madison, J. M., Druker, S., Olendzki, N., Magner, R., Reed, G., … & Carmody, J. (2012). Effect of mindfulness training on asthma quality of life and lung function: a randomised controlled trial. Thorax, 67(9), 769-776.
Platts-Mills, T. A. (2015). The allergy epidemics: 1870-2010. Journal of Allergy and Clinical Immunology, 136(1), 3-13.
Stein, S. W., & Thiel, C. G. (2017). The history of therapeutic aerosols: a chronological review. Journal of Aerosol Medicine and Pulmonary Drug Delivery, 30(1), 20-41.
Svenningsen, S., Kirby, M., Starr, D., Leary, D., Wheatley, A., Maksym, G. N., … & Parraga, G. (2013). Hyperpolarized 3He and 129Xe MRI: differences in asthma before bronchodilation. Journal of Magnetic Resonance Imaging, 38(6), 1521-1530.
Wenzel, S. E. (2012). Asthma phenotypes: the evolution from clinical to molecular approaches. Nature Medicine, 18(5), 716-725.