The Silent Killer Within : The Impact of Atherosclerosis
Cardiovascular diseases remain the leading cause of death worldwide, with atherosclerosis playing a pivotal role in their development. This insidious condition, often referred to as “hardening of the arteries,” is a complex process that develops over decades, silently damaging the arteries and setting the stage for potentially life-threatening events.
In this blog post, we’ll delve into the intricacies of atherosclerosis, exploring its causes, progression, and the cutting-edge research that offers hope for better prevention and treatment strategies.
Understanding Atherosclerosis: A Closer Look
Atherosclerosis is characterized by the accumulation of fatty deposits, known as plaques, within the inner lining of arteries (Wang et al., 2019). These plaques consist of cholesterol, fatty substances, cellular waste products, calcium, and fibrin. As they grow, they narrow the artery lumen, reducing blood flow to vital organs and tissues. More alarmingly, these plaques can rupture, triggering blood clot formation that can lead to heart attacks or strokes (Libby et al., 2019).
The process of atherosclerosis begins early in life, often in childhood or adolescence, and progresses slowly over many years. This gradual development makes it a particularly insidious threat, as symptoms may not manifest until significant damage has occurred.
The Risk Factors: What Sets the Stage for Atherosclerosis?
Understanding the risk factors for atherosclerosis is crucial for both prevention and early intervention. These factors can be broadly categorized into modifiable and non-modifiable risks:
Modifiable Risk Factors:
- High blood cholesterol levels, particularly LDL cholesterol
- Hypertension (high blood pressure)
- Smoking
- Obesity
- Physical inactivity
- Diabetes mellitus
- Poor diet high in saturated fats and trans fats
Non-modifiable Risk Factors:
- Age (risk increases with advancing age)
- Gender (men are at higher risk, though risk in women increases after menopause)
- Family history of cardiovascular disease
- Genetic predisposition
Research has shown that addressing modifiable risk factors can significantly reduce the risk of atherosclerosis progression. For instance, a large-scale study published in the New England Journal of Medicine demonstrated that intensive lifestyle changes, including a low-fat diet and regular exercise, could lead to regression of coronary atherosclerosis (Ornish et al., 1998).
The Silent Progression: How Atherosclerosis Develops
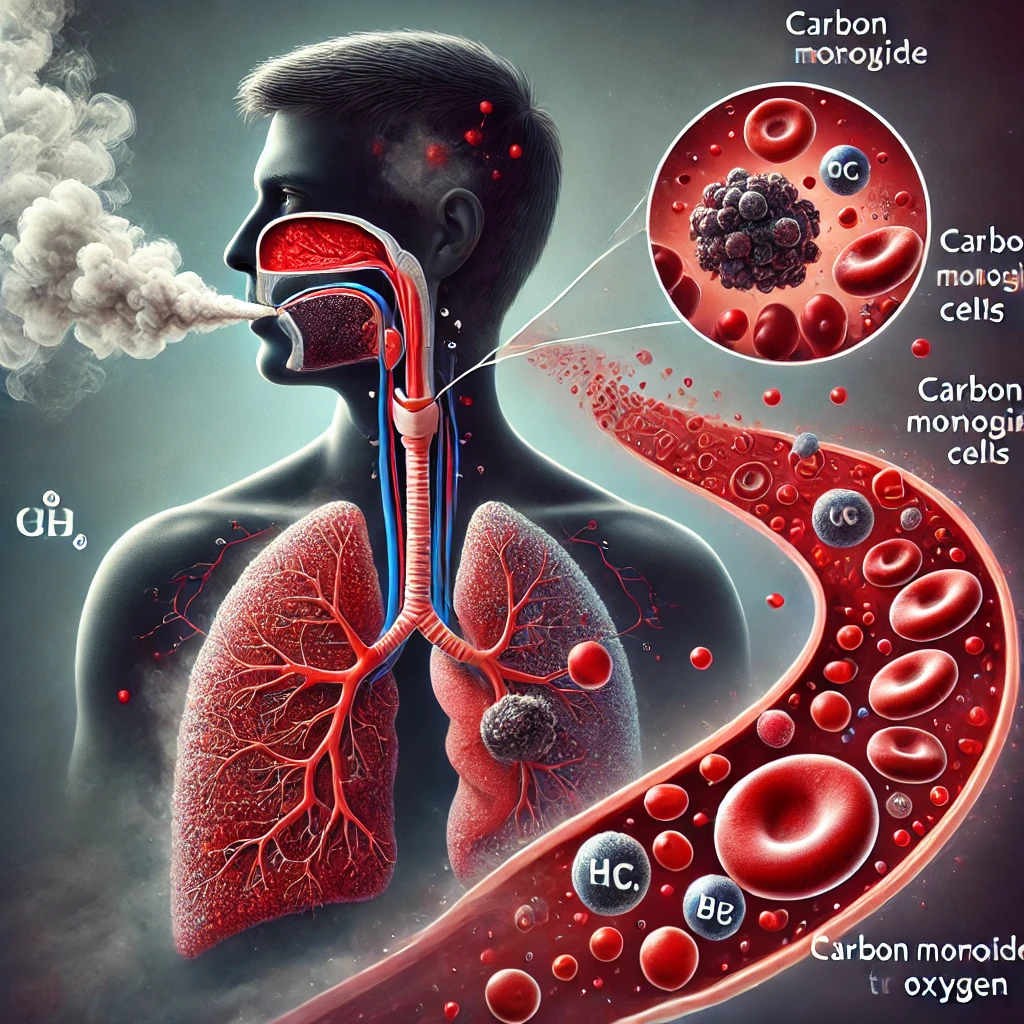
The development of atherosclerosis is a complex interplay of various biological processes. It begins with damage to the endothelium, the inner lining of arteries, which can be caused by factors such as high blood pressure, smoking, or high cholesterol levels. This damage allows LDL cholesterol particles to penetrate the artery wall, where they become oxidized and trigger an inflammatory response (Tabas & Lichtman, 2017).
As part of this response, white blood cells called monocytes enter the artery wall and transform into macrophages. These macrophages engulf the oxidized LDL particles, becoming foam cells in the process. Over time, these foam cells accumulate, forming the core of what will become an atherosclerotic plaque.
The body attempts to heal this damage by forming a fibrous cap over the developing plaque. However, this process can lead to further narrowing of the artery. Moreover, certain plaques, known as vulnerable plaques, have thin fibrous caps that are prone to rupture. When a plaque ruptures, it exposes its contents to the bloodstream, triggering rapid blood clot formation that can obstruct blood flow, potentially leading to a heart attack or stroke (Finn et al., 2010).
The Role of Inflammation: A Key Player in Atherosclerosis
Recent research has highlighted the crucial role of inflammation in the development and progression of atherosclerosis. While inflammation is a normal protective response of the body, chronic inflammation can contribute to various diseases, including atherosclerosis.
In the context of atherosclerosis, inflammation is both a cause and a consequence of plaque formation. The initial damage to the endothelium triggers an inflammatory response, which in turn promotes further plaque development. This creates a vicious cycle of inflammation and plaque growth (Ridker et al., 2017).
The recognition of inflammation’s role has led to new approaches in atherosclerosis treatment. For example, the CANTOS trial demonstrated that targeting inflammation with canakinumab, an anti-inflammatory drug, could reduce the risk of cardiovascular events in patients with a history of myocardial infarction (Ridker et al., 2017). This groundbreaking study opened up new avenues for atherosclerosis treatment beyond traditional lipid-lowering therapies.
Diagnosis and Monitoring: Catching Atherosclerosis Early
Given the silent nature of atherosclerosis progression, early detection is crucial. Several diagnostic tools and techniques are available to identify and monitor atherosclerosis:
- Coronary Calcium Scoring: This non-invasive CT scan can detect and quantify calcium deposits in coronary arteries, providing an early indication of atherosclerosis (Greenland et al., 2018).
- Carotid Intima-Media Thickness (CIMT) Test: This ultrasound-based test measures the thickness of the inner layers of the carotid artery, offering insights into atherosclerosis progression (Polak et al., 2011).
- Angiography: This invasive procedure involves injecting a contrast dye into the bloodstream and taking X-rays to visualize blood flow through the arteries, revealing any blockages or narrowing (Nørgaard et al., 2015).
- Intravascular Ultrasound (IVUS): This technique uses a small ultrasound probe inserted into the artery to provide detailed images of the arterial wall and any plaques present (Mintz et al., 2001).
- Optical Coherence Tomography (OCT): Similar to IVUS but using light instead of sound waves, OCT offers even higher resolution images of the arterial wall and plaques (Tearney et al., 2012).
These diagnostic tools, combined with regular health check-ups and monitoring of risk factors, can help in the early detection and management of atherosclerosis.
Combating Atherosclerosis: Prevention and Treatment Strategies
Prevention remains the cornerstone of atherosclerosis management. Lifestyle modifications play a crucial role in reducing risk and slowing progression:
- Healthy Diet: A diet rich in fruits, vegetables, whole grains, and lean proteins, while low in saturated fats and trans fats, can help maintain healthy cholesterol levels and reduce inflammation (Mozaffarian et al., 2011).
- Regular Exercise: Physical activity helps maintain a healthy weight, reduces blood pressure, and improves overall cardiovascular health (Lavie et al., 2015).
- Smoking Cessation: Quitting smoking can significantly reduce the risk of atherosclerosis progression and related cardiovascular events (Mons et al., 2015).
- Stress Management: Chronic stress can contribute to inflammation and other risk factors for atherosclerosis. Techniques such as mindfulness meditation have shown promise in reducing cardiovascular risk (Loucks et al., 2015).
For those already diagnosed with atherosclerosis or at high risk, medical interventions may be necessary:
- Statins: These cholesterol-lowering drugs have been shown to reduce cardiovascular events and mortality in patients with atherosclerosis (Collins et al., 2016).
- Antiplatelet Therapy: Drugs like aspirin can help prevent blood clot formation, reducing the risk of heart attacks and strokes (Antithrombotic Trialists’ Collaboration, 2009).
- PCSK9 Inhibitors: This newer class of drugs can dramatically lower LDL cholesterol levels and has shown promise in reducing cardiovascular events in high-risk patients (Sabatine et al., 2017).
- Revascularization Procedures: In cases of severe arterial narrowing, procedures such as angioplasty, stenting, or bypass surgery may be necessary to restore blood flow (Head et al., 2018).
The Future of Atherosclerosis Research and Treatment
As our understanding of atherosclerosis continues to evolve, new and exciting avenues for prevention and treatment are emerging:
- Targeted Anti-inflammatory Therapies: Building on the success of the CANTOS trial, researchers are exploring more specific anti-inflammatory approaches to treat atherosclerosis (Ridker, 2019).
- Nanotechnology: Nanoparticles are being developed to deliver drugs directly to atherosclerotic plaques, potentially improving efficacy while reducing side effects (Flores et al., 2019).
- Gene Therapy: Researchers are investigating ways to modify genes associated with atherosclerosis risk, offering the potential for more personalized prevention strategies (Zhao et al., 2019).
- Microbiome Modulation: Growing evidence suggests that the gut microbiome plays a role in atherosclerosis development. Manipulating the microbiome could offer new therapeutic approaches (Jie et al., 2017).
- Artificial Intelligence in Diagnosis: AI algorithms are being developed to analyze medical imaging data, potentially improving early detection and risk prediction for atherosclerosis (Dey et al., 2019).
Conclusion: A Call to Action
Atherosclerosis, the silent killer within our arteries, remains a significant health challenge. However, armed with a growing understanding of its mechanisms and an expanding arsenal of diagnostic and therapeutic tools, we are better equipped than ever to combat this disease.
The key lies in early prevention and proactive management. By adopting heart-healthy lifestyles, staying vigilant about our cardiovascular health, and leveraging the latest medical advancements, we can significantly reduce the burden of atherosclerosis and its potentially devastating consequences.
As research continues to unravel the complexities of this condition, there is hope for even more effective prevention and treatment strategies in the future. Until then, let us take charge of our cardiovascular health, making informed choices that can keep our arteries clear and our hearts strong for years to come.
Written by : Farokh Shabbir
References
Collins, R., Reith, C., Emberson, J., Armitage, J., Baigent, C., Blackwell, L., … & Peto, R. (2016). Interpretation of the evidence for the efficacy and safety of statin therapy. The Lancet, 388(10059), 2532-2561.
Dey, D., Slomka, P. J., Leeson, P., Comaniciu, D., Shrestha, S., Sengupta, P. P., & Marwick, T. H. (2019). Artificial intelligence in cardiovascular imaging: JACC state-of-the-art review. Journal of the American College of Cardiology, 73(11), 1317-1335.
Finn, A. V., Nakano, M., Narula, J., Kolodgie, F. D., & Virmani, R. (2010). Concept of vulnerable/unstable plaque. Arteriosclerosis, Thrombosis, and Vascular Biology, 30(7), 1282-1292.
Flores, A. M., Ye, J., Jarr, K. U., Hosseini-Nassab, N., Smith, B. R., & Leeper, N. J. (2019). Nanoparticle therapy for vascular diseases. Arteriosclerosis, Thrombosis, and Vascular Biology, 39(4), 635-646.
Greenland, P., Blaha, M. J., Budoff, M. J., Erbel, R., & Watson, K. E. (2018). Coronary calcium score and cardiovascular risk. Journal of the American College of Cardiology, 72(4), 434-447.
Head, S. J., Milojevic, M., Daemen, J., Ahn, J. M., Boersma, E., Christiansen, E. H., … & Kappetein, A. P. (2018). Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: A pooled analysis of individual patient data. The Lancet, 391(10124), 939-948.
Jie, Z., Xia, H., Zhong, S. L., Feng, Q., Li, S., Liang, S., … & Kristiansen, K. (2017). The gut microbiome in atherosclerotic cardiovascular disease. Nature Communications, 8(1), 845.
Lavie, C. J., Arena, R., Swift, D. L., Johannsen, N. M., Sui, X., Lee, D. C., … & Blair, S. N. (2015). Exercise and the cardiovascular system: Clinical science and cardiovascular outcomes. Circulation Research, 117(2), 207-219.
Libby, P., Buring, J. E., Badimon, L., Hansson, G. K., Deanfield, J., Bittencourt, M. S., … & Lewis, E. F. (2019). Atherosclerosis. Nature Reviews Disease Primers, 5(1), 1-18.
Loucks, E. B., Schuman-Olivier, Z., Britton, W. B., Fresco, D. M., Desbordes, G., Brewer, J. A., & Fulwiler, C. (2015). Mindfulness and cardiovascular disease risk: State of the evidence, plausible mechanisms, and theoretical framework. Current Cardiology Reports, 17(12), 112.
Mintz, G. S., Nissen, S. E., Anderson, W. D., Bailey, S. R., Erbel, R., Fitzgerald, P. J., … & Yock, P. G. (2001). American College of Cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound studies (IVUS). Journal of the American College of Cardiology, 37(5), 1478-1492.
Mons, U., Müezzinler, A., Gellert, C., Schöttker, B., Abnet, C. C., Bobak, M., … & Brenner, H. (2015). Impact of smoking and smoking cessation on cardiovascular events and mortality among older adults: Meta-analysis of individual participant data from prospective cohort studies of the CHANCES consortium. BMJ, 350, h1551.
Mozaffarian, D., Appel, L. J., & Van Horn, L. (2011). Components of a cardioprotective diet: New insights. Circulation, 123(24), 2870-2891.
Nørgaard, B. L., Leipsic, J., Gaur, S., Seneviratne, S., Ko, B. S., Ito, H., … & Achenbach, S. (2014). Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: The NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). Journal of the American College of Cardiology, 63(12), 1145-1155.
Ornish, D., Scherwitz, L. W., Billings, J. H., Brown, S. E., Gould, K. L., Merritt, T. A., … & Brand, R. J. (1998). Intensive lifestyle changes for reversal of coronary heart disease. JAMA, 280(23), 2001-2007.
Polak, J. F., Pencina, M. J., Pencina, K. M., O’Donnell, C. J., Wolf, P. A., & D’Agostino, R. B. (2011). Carotid-wall intima–media thickness and cardiovascular events. New England Journal of Medicine, 365(3), 213-221.
Ridker, P. M. (2019). Anticytokine Agents: Targeting Interleukin Signaling Pathways for the Treatment of Atherothrombosis. Circulation Research, 124(3),