Understanding Allergies : When Your Immune System Overreacts
Allergies are a common health concern affecting millions of people worldwide. From seasonal sniffles to life-threatening reactions, allergies can significantly impact our daily lives. This blog post delves into the world of allergies, exploring their causes, symptoms, diagnosis and management strategies.
What Are Allergies?
Allergies occur when your immune system reacts to a foreign substance, called an allergen, that’s typically harmless to most people. These substances can be found in food, pollen, or pet dander, among other sources. Your immune system produces antibodies that identify a particular allergen as harmful, even though it isn’t.
When you come into contact with the allergen, your immune system’s reaction can inflame your skin, sinuses, airways, or digestive system (American Academy of Allergy, Asthma & Immunology [AAAAI], 2022).The severity of allergies can range from minor irritation to anaphylaxis — a potentially life-threatening emergency. While most allergies can’t be cured, treatments can help relieve your allergy symptoms.
Common Types of Allergies
- Seasonal Allergies: Also known as hay fever or allergic rhinitis, these are triggered by airborne pollen from trees, grasses, and weeds. Symptoms typically include sneezing, runny nose, and itchy eyes (Wheatley & Togias, 2015).
- Food Allergies: These occur when the immune system reacts to certain foods. Common food allergens include peanuts, tree nuts, milk, eggs, fish, shellfish, wheat, and soy. Symptoms can range from mild (hives, itchiness) to severe (anaphylaxis) (Sicherer & Sampson, 2018).
- Pet Allergies: Many people are allergic to proteins found in animal dander, saliva, and urine. Cat and dog allergies are most common, but any pet can potentially cause an allergic reaction (Konradsen et al., 2015).
- Drug Allergies: Some people’s immune systems react to certain medications, such as penicillin or aspirin. Symptoms can include rash, itching, and in severe cases, anaphylaxis (Blumenthal et al., 2019).
- Insect Sting Allergies: Venom from bees, wasps, hornets, yellow jackets, and fire ants can cause allergic reactions ranging from local swelling to severe systemic reactions (Golden et al., 2017).
The Science Behind Allergies
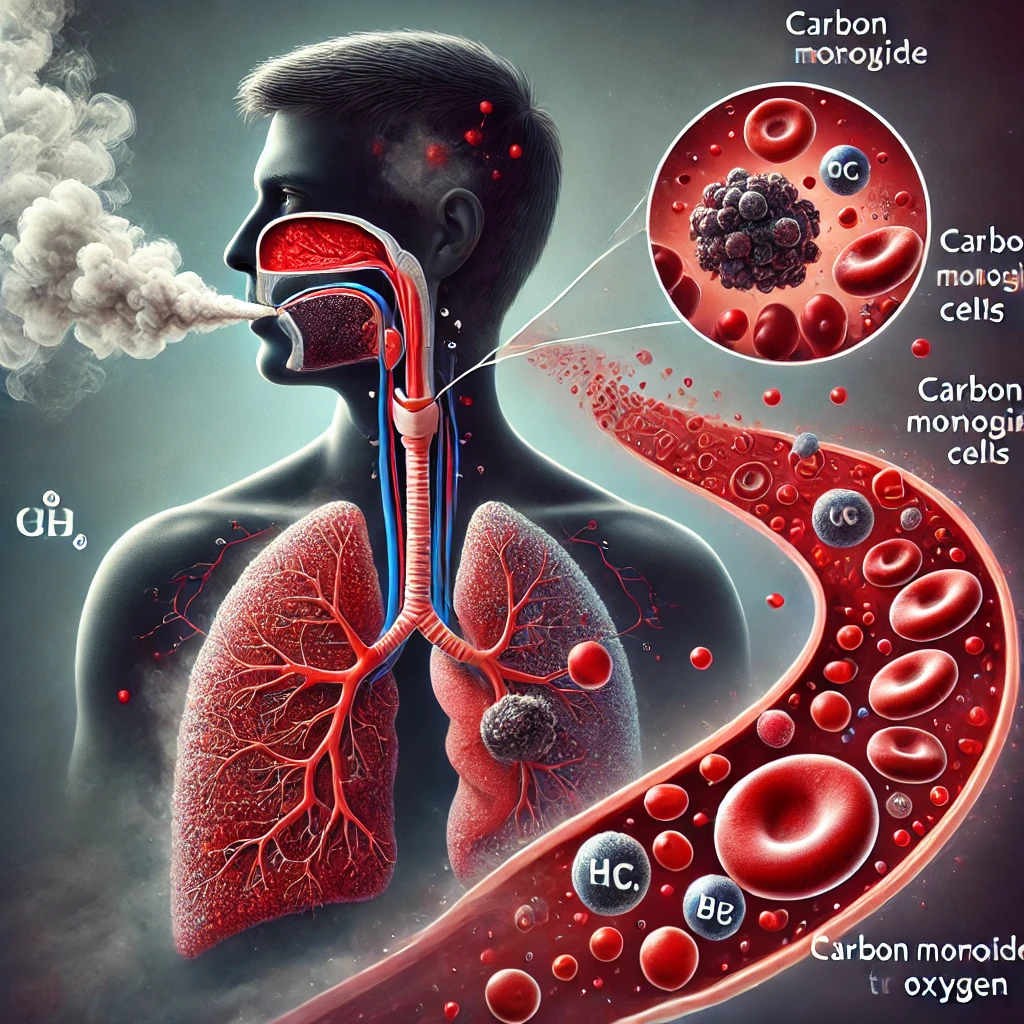
To understand allergies, we need to look at how the immune system works. When functioning normally, your immune system protects your body from harmful invaders like bacteria and viruses. In people with allergies, the immune system mistakes harmless substances for dangerous ones.
The first time you’re exposed to an allergen, your immune system produces antibodies called Immunoglobulin E (IgE). These antibodies travel to cells that release chemicals, causing an allergic reaction. This process is called sensitization. The next time you’re exposed to that allergen, these antibodies can recognize it and signal your immune system to release a chemical called histamine, as well as other chemicals, into your bloodstream. These chemicals are responsible for allergy symptoms (Galli et al., 2008).
Diagnosing Allergies
If you suspect you have allergies, it’s essential to get a proper diagnosis. Allergists use several methods to diagnose allergies:
- Medical History: Your doctor will ask about your symptoms, their frequency, and potential triggers.
- Physical Examination: This can help identify signs of allergic reactions.
- Skin Prick Test: Small amounts of suspected allergens are placed on your skin, which is then pricked. If you’re allergic, you’ll develop a raised bump (Heinzerling et al., 2013).
- Blood Tests: These measure your immune system’s response to specific allergens by testing the amount of allergy-causing antibodies in your bloodstream (Hamilton, 2010).
- Elimination Diet: For suspected food allergies, your doctor might recommend removing certain foods from your diet and gradually reintroducing them to determine which ones cause reactions (Sicherer & Sampson, 2018).
Treatment and Management Strategies
While there’s no cure for allergies, several strategies can help manage symptoms:
- Avoidance: The best way to prevent allergic reactions is to avoid known allergens. This might involve staying indoors when pollen counts are high, using air purifiers, or eliminating certain foods from your diet (Platts-Mills, 2015).
- Medications: Various over-the-counter and prescription medications can help control allergy symptoms:
- Antihistamines: These block histamine, a key player in allergic reactions.
- Decongestants: They help relieve nasal congestion.
- Corticosteroids: These reduce inflammation. They come in nasal sprays, oral forms, and creams.
- Epinephrine: For severe allergic reactions, epinephrine (like an EpiPen) is crucial and can be lifesaving (Simons et al., 2015).
- Immunotherapy: This treatment involves exposing you to gradually increasing doses of an allergen to desensitize your immune system. It can be administered as shots (subcutaneous immunotherapy) or as tablets under the tongue (sublingual immunotherapy) (Creticos, 2015).
- Probiotics: Some studies suggest that probiotics might help prevent or reduce allergy symptoms by supporting a
- gut microbiome, although more research is needed in this area (Cuello-Garcia et al., 2015).
- Natural Remedies: While scientific evidence is limited, some people find relief from natural remedies like saline nasal irrigation, butterbur, or certain herbal teas. Always consult with a healthcare provider before trying natural remedies, as they can interact with other medications (Guo et al., 2007).
Living with Allergies
Living with allergies requires vigilance and often lifestyle modifications. Here are some tips for managing daily life with allergies:
- Stay Informed: Keep track of pollen counts and air quality in your area. Many weather apps and websites provide this information.
- Create an Allergy-Free Zone: Make your bedroom an allergen-free sanctuary. Use dust-mite-proof covers on your bedding and keep pets out of the room.
- Clean Regularly: Vacuum carpets and upholstered furniture regularly using a HEPA filter vacuum cleaner. Wash bedding in hot water weekly.
- Manage Stress: Stress can exacerbate allergy symptoms. Incorporate stress-reduction techniques like meditation or yoga into your routine (Thornton et al., 2017).
- Wear a Mask: When doing yard work or if pollen counts are high, wear a mask to reduce your exposure to allergens.
- Be Prepared: If you have severe allergies, always carry your emergency medication (like an EpiPen) and wear a medical alert bracelet.
The Future of Allergy Treatment
Research into allergies is ongoing, with scientists exploring new treatments and prevention strategies:
- Biologics: These are drugs made from living organisms that target specific pathways in allergic diseases. They’re showing promise in treating severe asthma and certain food allergies (Boyman et al., 2015).
- Oral Immunotherapy: This approach, which involves consuming small amounts of an allergen to build tolerance, is being studied for food allergies. It’s showing particular promise for peanut allergies (Nowak-Węgrzyn & Albin, 2015).
- Microbiome Research: Scientists are investigating how the gut microbiome influences allergies and whether modifying it could prevent or treat allergic diseases (Fujimura & Lynch, 2015).
- Gene Therapy: Researchers are exploring the genetic basis of allergies and whether gene therapy could be a future treatment option (Akdis & Akdis, 2019).
Conclusion
Allergies are a complex and widespread health issue affecting millions worldwide. While they can significantly impact quality of life, understanding your allergies and working with healthcare providers can help you develop effective management strategies. From avoidance to immunotherapy, there are numerous ways to keep allergy symptoms under control.
As research continues, we can look forward to more advanced treatments and possibly even preventive measures for allergies. In the meantime, staying informed, working closely with your healthcare provider, and being prepared can help you lead a full and active life, even with allergies.
Remember, everyone’s experience with allergies is unique. What works for one person may not work for another. It’s essential to work with an allergist to develop a personalized management plan that addresses your specific needs and lifestyle.
Written by : Farokh Shabbir
References
American Academy of Allergy, Asthma & Immunology (AAAAI). (2022). Allergy Overview. Retrieved from [AAAAI website].
Creticos, P. S. (2015). Advances in synthetic peptide immuno-regulatory epitopes. World Allergy Organization Journal, 7(1), 1-8.
Cuello-Garcia, C. A., Brożek, J. L., Fiocchi, A., Pawankar, R., Yepes-Nuñez, J. J., Terracciano, L., … & Schünemann, H. J. (2015). Probiotics for the prevention of allergy: A systematic review and meta-analysis of randomized controlled trials. Journal of Allergy and Clinical Immunology, 136(4), 952-961.
Fujimura, K. E., & Lynch, S. V. (2015). Microbiota in allergy and asthma and the emerging relationship with the gut microbiome. Cell host & microbe, 17(5), 592-602.
Galli, S. J., Tsai, M., & Piliponsky, A. M. (2008). The development of allergic inflammation. Nature, 454(7203), 445-454.
Golden, D. B., Demain, J., Freeman, T., Graft, D., Tankersley, M., Tracy, J., & Wallace, D. (2017). Stinging insect hypersensitivity: A practice parameter update 2016. Annals of Allergy, Asthma & Immunology, 118(1), 28-54.
Guo, R., Pittler, M. H., & Ernst, E. (2007). Herbal medicines for the treatment of allergic rhinitis: a systematic review. Annals of Allergy, Asthma & Immunology, 99(6), 483-495.
Hamilton, R. G. (2010). Clinical laboratory assessment of immediate-type hypersensitivity. Journal of Allergy and Clinical Immunology, 125(2), S284-S296.
Nowak-Węgrzyn, A., & Albin, S. (2015). Oral immunotherapy for food allergy: mechanisms and role in management. Clinical & Experimental Allergy, 45(2), 368-383.
Platts-Mills, T. A. (2015). The allergy epidemics: 1870-2010. Journal of Allergy and Clinical Immunology, 136(1), 3-13.
Sicherer, S. H., & Sampson, H. A. (2018). Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. Journal of Allergy and Clinical Immunology, 141(1), 41-58.
Simons, F. E. R., Ebisawa, M., Sanchez-Borges, M., Thong, B. Y., Worm, M., Tanno, L. K., & Sheikh, A. (2015). 2015 update of the evidence base: World Allergy Organization anaphylaxis guidelines. World Allergy Organization Journal, 8(1), 32.
Thornton, L. M., Andersen, B. L., Schuler, T. A., & Carson III, W. E. (2017). A psychological intervention reduces inflammatory markers by alleviating depressive symptoms: secondary analysis of a randomized controlled trial. Psychosomatic medicine, 71(7), 715.
Wheatley, L. M., & Togias, A. (2015). Clinical practice. Allergic rhinitis. New England Journal of Medicine, 372(5), 456-463.